Health
Wait, How Often Do I Need A Pap Smear Again?
Doctors debunk nine myths about HPV & cervical cancer.
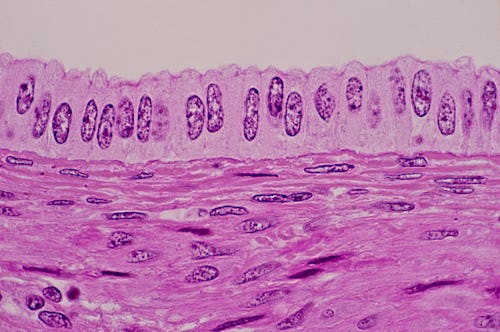
If you have a cervix, tests for human papilloma virus (HPV) and Pap smears have likely been part of your health checks since your early twenties. Uncomfortable though it can be to make small talk with a gynecologist who's extracting cells from your pelvis, check-ups are a key part of your health arsenal, up there with brushing your teeth and trying to eat vegetables once in a while. But HPV and its link to cervical cancer can attract a lot of myths and misconceptions.
Here are the basics. You can catch HPV through sexual intercourse — no, not through a toilet seat or being sneezed on. It's extremely common — something like 80% of people have it — and comes in many varieties, many completely benign. According to the World Health Organization, there are more than 100 types of HPV, only 14 of which have been linked to any kind of cancer — but the HPV vaccine, Gardasil 9, protects against nine of those strains. For around 44,000 people in the U.S. per year, the presence of certain HPV strains can spark the development of cervical, oral, anal or vulvar cancers.
If you do test positive for HPV, it's not the end of the world — and it's important to be able to navigate what the result means in terms of your cancer risk. Here are some things you might have heard about HPV and cervical cancer, sorted.
Myth 1: "You Need A Pap Smear Every Year"
You might associate your yearly OB-GYN appointment with the dreaded speculum. But new guidelines from the American Cancer Society say that actually, people should get an HPV test every five years after you turn 25, rather than a Pap smear once a year. If your OB-GYN doesn't have access to HPV testing, the ACS says, a Pap smear every three years works fine.The American College of Obstetricians and Gynecologists (ACOG), on the other hand, recommends people aged 21 to 29 get a Pap every three years, then do co-testing with a Pap and HPV test every five years from the age of 30 to 65, or a Pap every three years.
Pap smears and HPV tests are often given separately, though they involve the same process — having a sample taken from your cervix and tested. If you don't want to take up that much time at your doctor, though, co-testing does both tests at once.
The combined test, Dr. Christine Greves M.D., an OB-GYN at Orlando Health, tells Bustle, doesn't feel different to you at all. "You’ll still have a speculum exam to obtain cells from the cervix," she says. However, instead of putting the sample under a slide, it's put in a container that allows labs to look for a wide range of issues, including cervical cancer cells, pre-cancerous cell changes, and DNA or RNA from high-risk HPV strains. "As a patient, you won’t really notice a difference other than when getting your results," she says.
Dr. Naglaa Rizk M.D., an assistant professor of obstetrics, gynecology and women's health at Rutgers University and adviser to home testing company Everlywell, highly recommends combined tests because they give more information than the individual tests on their own, and new science agrees with her. A 2020 study of 13.6 million U.S. women published in the American Journal of Clinical Pathology found that co-testing was more effective than either Pap smears or HPV tests at detecting pre-cancers and aggressive cervical cancers.
“HPV co-testing is typically reserved for patients 30 years of age and older," Dr. G. Thomas Ruiz M.D., the lead OB-GYN at MemorialCare Orange Coast Medical Center, tells Bustle. "When results from a Pap smear are normal and HPV is negative, the person is low risk for cervical cancer over the next five years." So it's a good way to get all your testing done and dusted for a few years.
Myth 2: "Most People With HPV Get Cervical Cancer"
"Quite the opposite," Dr. Felice Gersh M.D., an OB-GYN, tells Bustle. "The vast majority of women catch HPV, and the vast majority of those women will control and suppress or eliminate it all by themselves, spontaneously!" Just two types, HPV 16 and 18, are responsible for around 70% of all cervical cancers and pre-cancerous lesions. The American Cancer Society, or ACS, notes that most people who are sexually active will contract HPV of one kind or another in their lives; data from the Centers for Disease Control & Prevention suggests that around 79 million Americans currently have at least one strain of HPV. It's hugely common and not a big deal. In fact, according to a study published in Viruses in 2017, around 80 to 90% of all HPV infections clear up on their own in two years.
Myth 3: "Cervical Cancer Is Common"
If you have HPV, developing cervical cancer is far from a certainty. "Cervical cancer is a deadly cancer and the overall U.S. survival rate is only 66%, but fortunately it is actually not a common cancer," Dr. Gersh says.
"The ACS estimates that 13,800 cases of invasive cervical cancer will be diagnosed this year alone — and that number doesn’t include pre-cancers, which are much more commonly diagnosed," Dr. Rizk says. Compared to the millions of people who have HPV, that's a very small number.
Myth 4: "Having Sex With A Woman Means You Can't Catch HPV"
HPV is spread by more than just penis-in-vagina sex. "HPV has been found in lesbians who have never had heterosexual intercourse with a man," Dr. Rizk says. "So if you have a cervix and you’re 21 or older, there are no excuses — be sure to talk to a doctor or nurse about your risk factors and get tested regularly." One study published in Sexually Transmitted Infections in 2017 actually found that non-heterosexual women were more likely to have HPV than heterosexual women.
Myth 5: "Men Can't Get Cancer From HPV"
This, OB-GYNs tell Bustle, is a dangerous myth. The CDC says that men can get anal and penile cancers from some HPV strains, and HPV is also linked to cancers in the back of the throat that appear in people of all genders. If you have HPV, you should tell your current sexual partner and encourage them to get tested, regardless of their gender.
Myth 6: "If You Have HPV, You'll Be Able To See It"
"If you have the type of HPV that causes warts, you may see it when there’s a wart, but other times it may not manifest," Dr. Greves says. "A woman may experience no symptoms and see no changes in her body, but can have HPV. That’s why seeing your doctor regularly as recommended is so important so we can catch it early."
Myth 7: "Pap Smears & HPV Tests Do The Same Thing"
Pap smears and HPV tests aren't the same. While both involve taking a sample from your cervix with a speculum and sending it off to be tested, they're looking for different things. Paps look for any kind of abnormal cells or signs in your cervix, but can't check your HPV status. HPV tests determine whether you've got HPV, and what kind. This is why you need to start getting both.
Myth 8: "You Don't Need HPV Tests If You've Had The HPV Vaccine"
This isn't true, Dr. Greves says. "The vaccine protects against four or nine HPV strains depending on the one you received," she says. "And there are other strains that can cause cervical cancer that aren’t covered in the vaccine, so get checked!" Dr. Rizk says that if you have a cervix and are over 21, you need to start getting screened for cervical cancer regularly.
Myth 9: "You Don't Need A Test If You Haven't Had Sex For A While"
Living the solitary life doesn't mean you can avoid testing. "Being sexually inactive or going through a 'dry spell' doesn’t mean you can skip your recommended HPV and cervical cancer screenings," Dr. Rizk says. "While having more partners does correlate with a higher risk of contracting HPV, it’s also possible to contract HPV after a single sexual encounter. And even if you haven’t had sex in a long time, you can actually experience HPV symptoms or complications weeks, months, or years after you contract the virus." Years of celibacy don't cancel out the risks of HPV, so you still need those tests.
The one time you can stop having Pap smears, according to OB-GYN Dr. Sherry Ross M.D., is if you're over 65 and have no history of pre-cancerous cervical cells. At that point, she says, you can remove the reminder from your calendar. Until then, your cervix needs a hero, and it's gotta be you.
Studies cited:
Kaufman, H.M., Alagia, D.P., Chen, Z., et al. (2020) Contributions of Liquid-Based (Papanicolaou) Cytology and Human Papillomavirus Testing in Cotesting for Detection of Cervical Cancer and Precancer in the United States, American Journal of Clinical Pathology, , aqaa074, https://doi.org/10.1093/ajcp/aqaa074
Liu, Z. C., Liu, W. D., Liu, Y. H., Ye, X. H., & Chen, S. D. (2015). Multiple Sexual Partners as a Potential Independent Risk Factor for Cervical Cancer: a Meta-analysis of Epidemiological Studies. Asian Pacific journal of cancer prevention : APJCP, 16(9), 3893–3900. https://doi.org/10.7314/apjcp.2015.16.9.3893
Reiter, P. L., & McRee, A. L. (2017). HPV infection among a population-based sample of sexual minority women from USA. Sexually transmitted infections, 93(1), 25–31. https://doi.org/10.1136/sextrans-2016-052536
Shanmugasundaram, S., & You, J. (2017). Targeting Persistent Human Papillomavirus Infection. Viruses, 9(8), 229. https://doi.org/10.3390/v9080229
Experts:
Dr. Felice Gersh M.D.
Dr. Christine Greves M.D.
Dr. Naglaa Rizk M.D.
Dr. Sherry Ross M.D.
Dr. G. Thomas Ruiz M.D.
This article was originally published on